Results in Minutes: How Rapid Point of Care Testing (POCT) is Transforming Diagnostics


SIGNALS+ NEWSLETTER SUBSCRIPTION
Stay updated and leverage Signals+ latest insights, information and ideas on Connectivity, Digital Health, Electrification, and Smart Industry.
Thank you for subscribing to ADI Signals+. A confirmation email has been sent to your inbox.
You'll soon receive timely updates on all the breakthrough technologies impacting human lives across the globe. Enjoy!
CloseRESULTS IN MINUTES: HOW RAPID POINT OF CARE TESTING (POCT) IS TRANSFORMING DIAGNOSTICS
August 10, 2022
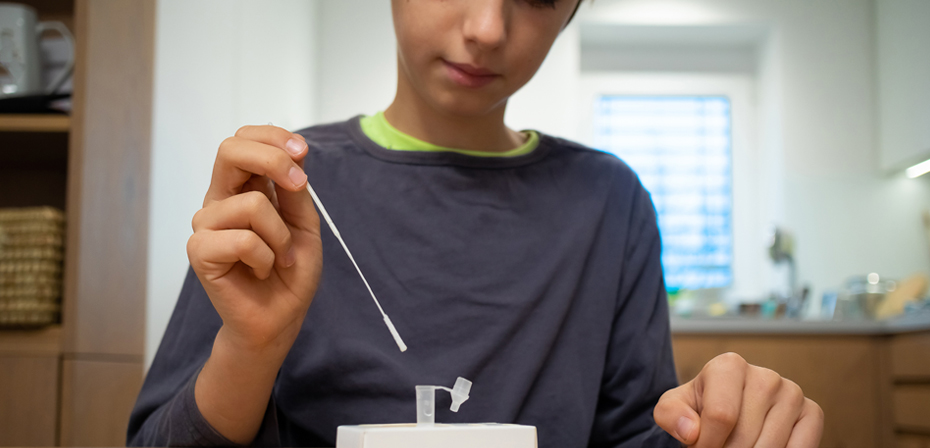
The COVID-19 experience has challenged the medical testing model and may have opened the door to a much broader array of at-home testing in the future.
Specific medical testing can be done at home, like pregnancy and the critical management of diabetes via glucose monitoring, but at-home testing options are still fairly limited in scope. Most medical testing begins at clinical points of care (POC) like hospitals and doctor’s offices, but the tests themselves are typically processed in centralized third party laboratories due to the size and complexity of the required devices and chemical reagents.
This model of healthcare is long established and familiar for patients; you see a medical professional who orders lab work. You then have a sample collected at a clinic or diagnostic testing facility and wait for results that are sent to a lab for processing. Depending on the test and the location of the lab, that wait could be a few hours or days.
$45 Billion
ESTIMATED SAVINGS FROM USING AT-HOME TESTING INSTEAD OF OFFICE VISITS.1
NOT ALL TESTS ARE CREATED EQUAL
The highly contagious nature of COVID-19 necessitated the ability to rapidly identify and quarantine infected individuals. While the need for widespread testing for COVID-19 was clear, it also quickly became apparent that each method of testing had its own set of benefits and drawbacks.
Tests performed in the lab setting typically use a molecular technique, such as PCR, that uses amplification prior to detecting the presence of the virus in the sample. This technique can detect very low levels of the virus, producing a highly sensitive result; however, patients typically wait 24 hours or more to receive these results.
While rapid home tests can give you results in 15 minutes, rather than a day or more, they are typically less accurate, as they rely on antigens or antibodies. But there is no amplification process in an antigen or antibody test, meaning they are significantly less sensitive. This testing technique gives you results faster than molecular, but the patient’s viral load needs to be high enough to meet the limit of detection, creating a delay from exposure to a positive result. The benefit of getting a result in 15 minutes at home is significantly reduced if that result cannot be relied upon.
THE EVOLUTION OF INFECTIOUS DISEASE TESTING AT HOME
With these learnings in hand, testing manufacturers are turning their attention to creating smaller, automated, cost-effective versions of the lab-based PCR technique and similar molecular methods. Such devices would help evolve the medical testing landscape from its current centralized model to one that is more distributed.
In parallel, rapid test manufacturers are now looking to expand their point of care testing (POCT) offerings to include other highly contagious, damaging, and potentially deadly viruses like STDs or the flu.
Imagine the scenario where you wake up with a sore throat and runny nose one morning. Is it the flu? The common cold? COVID? Or is it just the result of sleeping with a window open? To find an answer, you would need to visit a clinic. By the time you choose to do so, you may have infected multiple people.


Rapid point-of-care testing can provide results in minutes, helping to enable the potential for quicker clinical decision making, to decrease costs, and to improve patients’ quality of life.
“Imagine a single test that could, in one sample, simultaneously check for the presence of several viruses with similar symptoms and return a lab-quality result in your own home or local doctors office.”
Now, imagine a single test that could simultaneously check for the presence of several viruses with similar symptoms and return a lab-quality result in your own home. It is easy to see the impact such a product could have, not only in eliminating barriers to testing but also in altering the trajectory of infection spread in future flu seasons. Multi-pathogen molecular testing is the holy grail of point of care medical testing.
FLEXIBILITY IS THE KEY
The market is exploring multitarget tests that can diagnose different viruses with similar symptoms. The key to its success will be building the testing devices in such a way that they can easily adapt over time as additional assays are added. This approach not only allows manufacturers to quickly react when a new virus emerges but also removes the need for multiple rounds of regulatory approvals: The multifunction test system will go to the Federal Drug Administration as a single review package, rather than each individual new assay requiring its own instrument approval.
One opportunity for multi-pathogen testing is in clinical settings like doctor offices or walk-in clinics. The benefit is two-fold: These types of medical facilities are often space-constrained, making a single, multifunctional, printer-sized device an attractive option. It is also helpful to time-constrained clinical staff who will only need to learn and use a single device, rather than remembering the order of operations on dozens.
This approach is also uniquely beneficial in the sexual health space. Offering a multi-disease STD tester at the point of care would provide space and convenience benefits. It would also allow physicians to diagnose and prescribe treatment in a single visit, rather than requiring a follow-up. This is of particular importance in the sexual health space where studies suggest up to half of patients who are notified of a positive test result may not return for treatment.
DELIVERING ON THE PROMISE OF MULTI-DISEASE TESTING SYSTEMS
While the opportunity is clear for testing manufacturers, the path to get there is onerous. Measurement and sensing expertise will be critical, and these companies are specialists in chemistry, not electronics and complex signal chains. So while recognizing the signature of a virus may come quickly, building products such as a potentiostat or high sensitivity fluorescence detector will take longer.
The solutions these manufacturers design using discrete components, like those on the market today, will require more components and greater size and also be more expensive and less flexible than integrated, software-defined solutions.
Partnering with a company like Analog Devices—whose expertise encompasses both discrete and integrated, precision optical and electrochemical solutions—can help testing providers focus on what they do best: the science. Meanwhile, the IC partner delivers integrated, future-proofed solutions that help them to get to market faster, at lower cost, and with superior offerings that can rapidly adapt to shifting market needs.

One real-life example of this kind of partnership is within the blood glucose monitoring (BGM) space. ADI worked with Roche Diabetes Care to develop a next-generation electrochemical BGM platform that was recognized by the National Library of Medicine for exceeding international accuracy standards.2
The electrochemical impedance technology improved the monitor’s accuracy by reducing the influence of outside factors like temperature, ambient humidity, and interferences present in the blood. This approach can easily translate to improved outcomes in infectious disease.
“Partnering with a company like Analog Devices—whose expertise encompasses both discrete and integrated, precision optical and electrochemical solutions—can help testing providers focus on what they do best: the science.”
KNOWLEDGE IS POWER
Having a single test that can return meaningful results for multiple ailments is an exciting concept. It has the potential to play a critical preventative role in the spread of infection and in optimizing daily management of a variety of chronic conditions. It can even help in optimizing everyday health, like understanding your body’s unique vitamin and mineral needs over time, creating opportunities to turn testing toward maintaining good health rather than just monitoring illness.
Multi-pathogen testing can also reduce the burden on overbooked clinics and other points of care and decrease the volume of samples to be processed by labs. It will also play an enormous role in population health, giving people rapid answers to whether they are sick and should stay home or healthy but need to take an allergy pill.
Additionally, the barriers to testing have come down. While someone may think twice about taking the time to make an appointment and be tested at a nearby point of care, there’s hardly any reason not to do a quick swab at home to confirm you’re healthy before attending your morning yoga class or an indoor family gathering.
DEMOCRATIZING PREVENTATIVE CARE
Multi-disease testing units that are small, flexible, affordable, and easy to use will give people more than just knowledge and reassurance—they can give both access and agency to you and your family to make decisions that benefit your health and wellbeing. The Center for Workforce Health and Performance noted that if people took care of more of their healthcare needs at home, this could result in an estimated $45 billion saved from unneeded doctors’ visits.
Who would have thought we could thank a global pandemic for opening the door to better individual and population health overall and greater access to healthcare for underserved populations?

References
1CWHP | Research to Practice (tcwhp.org)
2National Library of Medicine





 Close Details
Close Details

